📈 Global Knee Relacement Surgery Rates
- An international survey covering 18 countries estimated that there are ~ 1,324,000 total (primary + revision) knee replacement procedures per year across a population of ~ 755 million. PMC+2PubMed+2
- In that survey, the combined rate (primary + revision) averaged 175 procedures per 100,000 population per year, with a median of 149/100,000. PMC+1
- The rate varied widely between countries — from as low as ~ 8.8 per 100,000 to as high as ~ 234 per 100,000, change on the country. PMC+1
- According to recent data from organizations that record joint replacements (registries), in one country the 2023 volume of primary knee replacement procedures reached a new annual high. ncbi.nlm.nih.gov+1
- In many developed countries, knee (and hip) replacements have become among the most commonly performed elective orthopedic surgeries. OECD+2OECD+2
👥 Prevalence in populations / Living with Knee Replacements
- In the United States (as of data around 2010), about 1.52% of the overall population had had a total knee replacement, corresponding to about 4.7 million people. PMC+1
- Among adults aged 50 or older in the U.S., estimates suggest about 4.2% (95% CI: 3.7%–4.6%) currently live with a knee replacement (primary or revised). PMC+1
- By sex and age: prevalence in older age groups increases sharply. For instance, for those 80 years old, prevalence reached ~ 10.38% (for total knee replacement). PMC+1
🕰️ Trends over time & Projected Growth
- Over past decades, usage of TKR has grown significantly — in many countries demand has increased as populations age, obesity rises and osteoarthritis becomes more common. PMC+2OECD+2
- A systematic review of national joint-replacement registries found that from 2010 to 2023, the incidence of TKR increased substantially and projections suggest further growth of at least 130% in many countries in coming decades. PubMed+1
- This means health systems will likely see many more knee replacements in the future — with consequences for planning surgical capacity, long-term care and follow-up. PubMed+1
🧾 Longevity & Revision: How Long Replacements Last / Need for Revision?
- Long-term data from large registries indicate that about 82% of total knee replacements remain functional at 25 years after surgery (for total knee; partial/unicompartmental ones have lower long-term survival). NIHR Evidence+2Bristol Health Partners+2
- More specifically: about 93% of total knee replacements function at 15 years, 90% at 20 years and 82% at 25 years. Bristol Health Partners+2News-Medical+2
- But revision surgery is sometimes needed. In one large cohort study: for TKR, 10-year prosthesis survival was ~ 96.1%, but 20-year survival dropped to ~ 89.7%. PubMed+1
- Risk of needing revision depends strongly on age at first surgery: patients who received knee replacements younger than 70 years had a much higher lifetime revision risk — up to ~ 35% in some groups (especially men in early 50s). PubMed
- Common reasons for revision: loosening of the implant (aseptic/mechanical), wear (plastic or bone-prosthesis interface), infection, instability or progressive joint problems. anatolianjmed.org+1
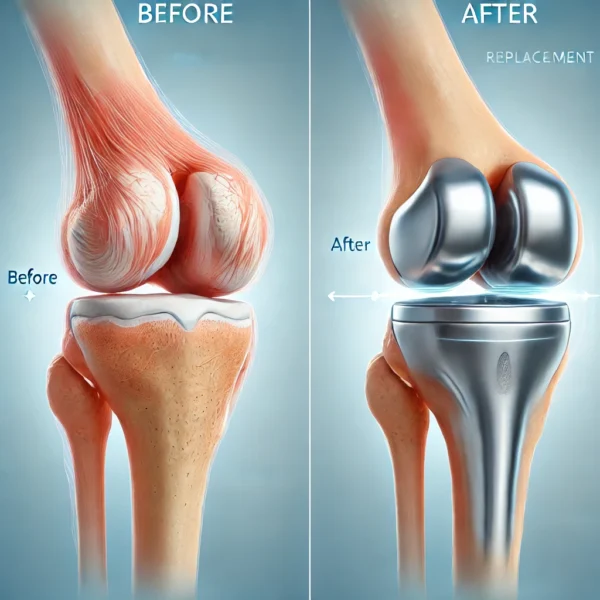
✅ Who Needs a Knee Replacement?
A knee replacement is usually recommended for advanced, long-term knee damage that no longer improves with non-surgical treatments.
✔ Most Common Condition
- Severe knee osteoarthritis
- Especially when cartilage is completely worn out (“bone-on-bone”)
✔ Other Conditions That Lead to Knee Replacement
- Rheumatoid arthritis or other inflammatory joint diseases
- Post-traumatic arthritis after fractures or ligament injuries
- Avascular necrosis (loss of blood supply causing bone collapse)
- Severe deformity (bow-legs ➝ varus or knock-knee ➝ valgus)
- Failed previous knee surgeries (e.g., failed meniscus or ligament reconstructions)
🧍 Symptoms Indicating Someone May Need a Knee Replacement
Someone is considered a candidate if they have:
| Symptom / Problem | Description |
|---|---|
| Severe knee pain | Pain even at rest, including nighttime pain |
| Limited mobility | Difficulty walking, stairs, standing up |
| Chronic swelling & stiffness | Persistent inflammation affecting movement |
| Grinding / crunching sensation | Due to bone rubbing on bone (cartilage loss) |
| Knee giving out / instability | Feels like it may collapse |
| Severe deformity | Bow-leg / knock-knee changes visible |
| Quality of life reduced | Can’t do daily activities or work normally |
🏥 When Conservative Treatment No Longer Works
You are considered a surgical candidate if non-surgical options have failed, such as:
- Pain medications & anti-inflammatories
- Corticosteroid or hyaluronic acid injections
- Weight reduction programs
- Physiotherapy / strengthening exercises
- Knee braces
- Platelet-rich plasma (PRP) injections
- Lifestyle modifications & activity changes
If these do not relieve symptoms anymore and X-rays show advanced cartilage damage, surgery becomes the best option.
🔍 Age Considerations
- Typically between 55–80 years old but younger patients sometimes need it
- Younger than 50–55 can get knee replacements but have:
- Higher revision rates
- Implants may wear out sooner
- More physical expectations
Elderly patients (>80) may still benefit if overall health is good.
💡 Ideal Candidate Profile
A person most likely to benefit from knee replacement usually shows:
- Severe structural joint damage
- Major pain not improved by other treatments
- Major limitation in mobility and independence
- Desire to remain active
❌ Who Should Delay or Avoid Surgery
A knee replacement might be postponed if the patient:
- Has active infection
- Has uncontrolled diabetes or heart issues
- Has severe obesity (BMI > 40 increases risks)
- Has untreated vascular issues in the leg
✅ Success Rates & Longevity of Implants
- Many large-scale studies and registries find that ≈ 90–95% of total knee replacements are still working well at 10 years. Factually+2PubMed+2
- For longer-term durability: about 82% of TKR implants remain functional at 25 years. NIHR Evidence+1
- A study of 5,649 primary total knee arthroplasties (TKAs) showed a 94.2% survival rate at 25 years and 92.4% at 30 years follow-up. PubMed
- More recent mid-term data: one implant system had a 5-year survival rate of 99.2% (i.e. almost all implants still in place 5 years after surgery). anatolianjmed.org+1
- Functional outcomes are also generally good: in one 10-year follow-up study, patients had good/excellent functional and satisfaction scores with aseptic (non-infection) implant survival at 99%. PubMed
What this means: For most people, knee replacement offers long-lasting relief and improved function — many implants last 2–3 decades. It remains one of the most successful and durable orthopedic surgeries long-term.
⚠️ Common Complications & Risks After Knee Replacement
Although generally safe and effective, TKR carries some risks — both short-term (postoperative) and long-term (implant-related). Key complications include:
| Complication / Problem | Frequency / Details / Risk Factors |
|---|---|
| Revision surgery (implant failure / need for reoperation) | Meta-analysis: ~ 4.4% revision rate after average 10.7 years follow-up. PubMed Revision risk is higher if the patient was younger (< 60 years) at time of surgery or if cementless implants used. PubMed+1 |
| Aseptic loosening (mechanical failure, wear, bone-prosthesis interface issues) | Among causes of revision: aseptic loosening accounted for ~ 31% in a meta-analysis. PubMed Other long-term causes: polyethylene wear, osteolysis, instability, malalignment. anatolianjmed.org+2anatolianjmed.org+2 |
| Infection (prosthetic joint infection) | Though rare, infection remains a serious complication. Healthline+1 |
| Other mechanical problems (implant wear, patellar issues, instability, fractures around prosthesis) | Reported among revision causes: e.g. patellar problems ~14%, polyethylene wear ~16%, etc. PubMed+1 |
| Complications in high-risk groups (e.g. patients with bleeding disorders)** | For example, in people with hemophilia undergoing TKR, complication rates are high (7-30%) and 10-yr prosthesis survival is lower (~80–90%) compared to general population. MDPI |
In addition, short-term postoperative risks (though generally low) can include infection, blood clots, stiffness, reduced mobility or need for revision, depending on patient health, surgical technique and rehabilitation. Healthline+2anatolianjmed.org+2
🎯 What “Success” Usually Means — And What It Doesn’t Guarantee?
Success in knee replacement typically means:
- The implant remains in place (no revision)
- Pain is relieved or significantly reduced
- Knee function (mobility, walking, daily activities) improves
But even with a “successful” implant:
- Some patients — estimates vary — may still experience residual pain, stiffness or limited range of motion. A pooled review notes that up to ~20% of patients might not be fully satisfied despite a functioning TKR. Factually+1
- Implant longevity depends heavily on factors like age, weight, activity level, surgical technique and implant type. Younger or more active patients tend to have higher revision rates. PubMed+1
- Long-term wear (plastic parts, bone-implant interface) plus biological responses (bone loss, loosening) can eventually lead to failure. anatolianjmed.org+1
📊 Summary — What You Can Tell Patients/Patients-to-be?
- Knee replacement is highly effective, with 90–95% implant survival at 10 years and many implants lasting 20–25 years or more.
- Most patients experience significant pain relief and improved mobility.
- Risk of revision is relatively low but increases in younger, more active patients or with certain implant types or comorbidities.
- Complications — especially loosening, wear, infection — remain possible, so long-term follow-up and proper rehab are important.
- Even when “successful,” a minority of patients may still have some discomfort, stiffness or less-than-perfect function.
🗓️ Knee Replacement Recovery Timeline
⏱️ Total healing time: 6–12 months
- Most function + pain relief: 3 months
- Full strength + best mobility: 9–12 months
📍 Day 1–Week 1: Immediate Post-Op Phase
| Time | What Happens |
|---|---|
| Day of surgery | Stand with assistance, begin walking with walker/crutches |
| Day 1–3 | Start physical therapy: leg lifts, ankle pumps, bending exercises |
| Pain & swelling | High but controlled with medication & ice |
| Movement goals | Bend knee to ≈ 60–70°, straighten fully |
| Stitches | Remain in; bandage daily check |
✔ You go home 1–3 days after surgery (sometimes same-day discharge).
📍 Week 2–Week 6: Early Recovery
| Period | What Happens |
|---|---|
| 2 weeks | Stitches removed, swelling still normal |
| 4 weeks | Walking with cane instead of walker |
| 6 weeks | Drive if off strong pain meds and can bend knee safely |
| Pain | Still present but improving |
🎯 Goals by Week 6
- 90–100° knee bend (flexion)
- Walk household distances without major help
- Reduce pain & swelling
📍 Week 6–3 Months: Functional Recovery
| Period | Key Progress |
|---|---|
| 6–8 weeks | Most patients walk without cane |
| 10 weeks | Climb stairs more comfortably |
| 3 months | Return to work (desk jobs common), longer walks |
🎯 Goals by Month 3
- 110–120° knee bend
- Walk normally without limp
- Return to normal daily activity
Pain level: greatly reduced
Stiffness: still common, especially morning/evening
📍 3–6 Months: Strength & Mobility Gain
| Period | What improves |
|---|---|
| 3–4 months | Return to light sport (swimming, cycling, treadmill) |
| 4–6 months | Most patients report major pain relief |
✔ Kneeling may still feel uncomfortable
✔ Some swelling can appear at night after active days
📍 6–12 Months: Full Recovery
| Period | What Happens |
|---|---|
| 6 months | Knee feels “almost normal” for majority |
| 9–12 months | Best strength, balance & mobility achieved |
| 1 year | Full healing of bone + scar tissue flexibility |
After 1 year:
- Can resume most low-impact sports
- Very low pain levels
- Maximum motion achieved
🏃 Activities: What You Can & Cannot Do
👍 Safe / Recommended
- Walking
- Cycling
- Swimming
- Low-resistance treadmill
- Yoga (gentle)
- Elliptical
⚠️ Avoid long-term
(because they wear out implants faster)
- Running
- Jumping / High impact aerobics
- Deep squatting with weight
- Competitive high-impact sports (basketball, football)
💡 Expected Feelings by Stage
| Time | How the Knee Feels |
|---|---|
| 1–2 weeks | sore, stiff, swollen, limited sleep comfort |
| 1 month | less pain, improving flexibility |
| 3 months | daily activities feel easier |
| 6 months | strong, low pain, better stability |
| 12 months | fully functional, minimal stiffness |
🚨 When to Call Doctor? (Red Flags)
- Fever > 38°C
- Sudden extreme pain after being stable
- Increased redness, warmth, pus at incision
- Chest pain or breathing trouble (possible clot)
- Calf pain + swelling (possible DVT)
🌟 Summary
- Return to home walking: 1–3 weeks
- Drive: 4–6 weeks
- Work (desk job): 6–8 weeks
- Full mobility & strength: 6–12 months
- Best walking comfort: 3 months
- Highest implant durability achieved: around 1 year
🌍 International Cost Comparison Of Knee Replacement
| Country / Region | Approximate Cost (Unilateral Total Knee Replacement) |
|---|---|
| United States (private) | ≈ US $35,000 medcureasia.com+2PlacidWay+2 |
| Germany | ≈ US $21,000 medcureasia.com |
| United Kingdom (private) | ≈ US $23,000–$25,000 medcureasia.com+1 |
| Turkey (private / self-pay / medical-tourism) | ≈ US $6,600–$11,000 (common quoted range: €6,000–€10,000) MedicalTourism.Review+1 |
| India | ≈ US $4,500–$8,000 typical for quality hospitals. Lower-cost baseline around US $3,600–6,000 in some centers. MediGence+1 |
We wish a healthy and happy life to you. You can find details about a great options for hearing problems below link: Stapedectomy Surgery.




