What is Amniotic Fluid Embolism?
Amniotic fluid embolism is a rare but serious condition that happens when amniotic fluid (the fluid surrounding a baby in the womb), fetal cells or other debris enter the mother’s bloodstream during labor, delivery or shortly after.
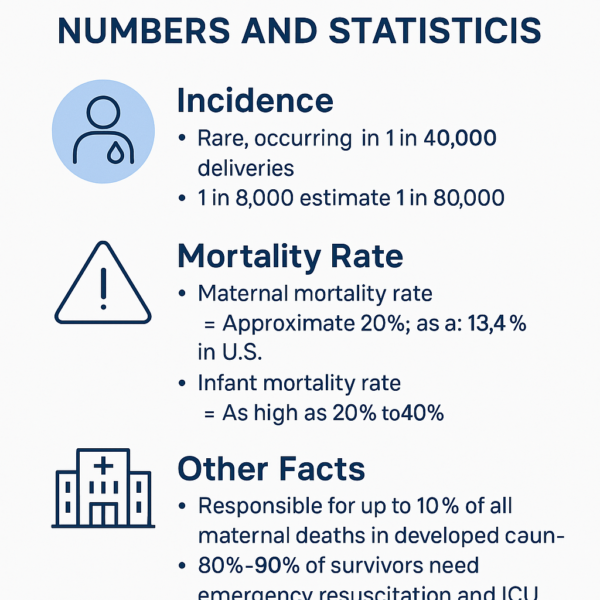
Numbers And Statistics of Amniotic Fluid Embolism
🧮 Incidence
- AFE is rare, occurring in about:
- 1 in 40,000 deliveries worldwide
- Estimates range from 1 in 8,000 to 1 in 80,000 depending on the country and how cases are reported
⚠️ Mortality Rate
- Maternal mortality (death) rate:
- Around 20% to 60%
- In the U.S., it’s approximately 13.4% (with modern medical care)
- Infant mortality rate:
- As high as 20% to 40%, often due to lack of oxygen during the event
🏥 Other Facts
- AFE is responsible for up to 10% of all maternal deaths in developed countries.
- Survivors often require intensive care:
- 80%–90% of survivors need emergency resuscitation and ICU support
- Long-term complications include brain injury or organ damage due to lack of oxygen
What Are The Causes Of Amniotic Fluid Embolism?
⚠️ Main Risk Factors & Triggers
1. Labor and Delivery (Most Common Time)
- The stress and force of labor may allow fetal material to enter the mother’s bloodstream.
- Can occur during:
- Normal vaginal birth
- Cesarean section (C-section)
- Immediately after delivery
2. Uterine or Cervical Trauma
- Any physical injury or tearing in the uterus or cervix can provide an entryway for amniotic fluid into the bloodstream.
- Tears during labor
- Manual removal of placenta
- Uterine rupture (rare but serious)
3. Abnormal Placental Conditions
- Placenta previa – placenta covers the cervix, increasing the chance of bleeding and injury during delivery.
- Placental abruption – placenta detaches from the uterine wall too early, disrupting the barrier between maternal and fetal blood.
4. Medical Interventions
Invasive procedures may unintentionally introduce amniotic components into circulation:
- Amniocentesis – needle insertion into the uterus to collect amniotic fluid
- Intrauterine pressure catheters
- Induced labor, especially with strong uterotonics like oxytocin or prostaglandins
5. High-Intensity Uterine Contractions
- Overstimulation of the uterus may force amniotic fluid into the bloodstream.
- More likely during induced labor or when labor progresses very rapidly.
6. Multiple Pregnancies (Twins, Triplets, etc.)
- Higher volume of amniotic fluid and more strain on the uterus increase risk.
7. Advanced Maternal Age
- Women over age 35 may have a slightly higher risk, possibly due to higher chance of complicated deliveries.
What Are The Symptoms Of Amniotic Fluid Embolism?
🚨 Main Symptoms of Amniotic Fluid Embolism
1. Sudden Difficulty Breathing (Respiratory Distress)
- Gasping for air
- Shortness of breath
- Rapid breathing (tachypnea)
- Cyanosis (blue lips or skin due to low oxygen)
2. Sudden Drop in Blood Pressure (Hypotension)
- Leads to shock
- Dizziness or fainting
- Weak pulse
- Cold, clammy skin
3. Heart Problems
- Irregular heart rate (arrhythmia)
- Cardiac arrest (heart stops beating)
- Chest pain
4. Altered Mental Status
- Confusion
- Seizures
- Unconsciousness or coma
5. Excessive Bleeding (Disseminated Intravascular Coagulation – DIC)
- Severe vaginal bleeding
- Bleeding from IV sites, surgical incisions, or mucous membranes
- Blood clotting problems
6. Other Symptoms
- Nausea or vomiting
- Restlessness or agitation
- Fetal distress (abnormal heart rate in the baby)
⏱️ Timeline of Symptoms
- Phase 1 – Respiratory and Cardiac Collapse
- Sudden breathing trouble, low blood pressure, and heart problems
- Phase 2 – Hemorrhagic Phase
- If the mother survives the initial collapse, she may enter a phase of massive bleeding and clotting failure (DIC)
How To Detect Amniotic Fluid Embolism?
🧪 Diagnosis of Amniotic Fluid Embolism
⚠️ Key Point: AFE Is a Clinical Diagnosis
There is no single test that can confirm amniotic fluid embolism. It is diagnosed based on sudden symptoms and by ruling out other possible causes.
🩺 How Doctors Diagnose AFE
1. Clinical Observation
- Sudden difficulty breathing
- Low blood pressure or shock
- Seizures or loss of consciousness
- Excessive bleeding (DIC) These signs usually occur during labor, delivery or shortly after.
2. Ruling Out Other Conditions
Because AFE symptoms mimic other emergencies, doctors must quickly exclude:
- Pulmonary embolism
- Severe allergic reaction (anaphylaxis)
- Heart attack
- Eclampsia (seizures from high blood pressure)
- Sepsis (severe infection)
- Uterine rupture
3. Lab Tests (Supportive, Not Confirmatory)
While no test can confirm AFE, these can help detect related problems:
- Blood gases – show low oxygen levels
- Complete blood count (CBC) – may show abnormal clotting or low platelets
- Coagulation tests (PT, aPTT, fibrinogen) – help identify DIC (bleeding disorder)
- Chest X-ray or echocardiogram – may show fluid in the lungs or heart dysfunction
4. Amniotic Fluid Components in the Blood (Rarely Used)
- Tests can sometimes detect fetal cells, lanugo or squamous cells in the mother’s blood or lungs
- These findings are not always present and are not required for diagnosis
🧠 Diagnostic Criteria (Used in Research & Practice)
- Sudden cardiorespiratory collapse
- Evidence of DIC (bleeding disorder)
- Symptoms during labor or within 30 minutes postpartum
- No other explanation for the symptoms
📋 Summary:
Amniotic fluid embolism is diagnosed based on: ✅ Sudden symptoms during labor or delivery
✅ Excluding other emergencies
✅ Lab and imaging tests that support, but don’t confirm the diagnosis
🩺 Treatment of Amniotic Fluid Embolism
⚠️ Emergency, Life-Saving Care
Amniotic fluid embolism is a medical emergency that requires immediate intervention by a full medical team—usually in a delivery room or ICU. Since AFE progresses rapidly, stabilizing the mother and protecting the baby (if still in utero) are top priorities.
🛑 Step 1: Stabilize Heart and Lungs
- Oxygen Therapy
- High-flow oxygen via mask or mechanical ventilation (if needed)
- CPR (Cardiopulmonary Resuscitation)
- If the heart stops, immediate resuscitation is needed
- Intubation and Mechanical Ventilation
- Used if breathing is inadequate or the patient is unconscious
- Vasopressors
- Medications (like epinephrine or norepinephrine) to raise dangerously low blood pressure
🩸 Step 2: Control Bleeding and Correct Coagulation (DIC)
- Blood Transfusions
- Red blood cells, platelets, plasma (to replace what’s lost)
- Clotting Factors
- Fresh frozen plasma, cryoprecipitate or fibrinogen concentrates
- Medications to Help Blood Clot
- Sometimes drugs like tranexamic acid are used
- Monitor for Organ Failure
- Kidneys, liver, and other organs may need support (e.g., dialysis)
👶 Step 3: Emergency Delivery (If the Baby Is Still Inside)
- Immediate C-section may be performed if the mother is unstable and the baby is in distress.
- This also helps improve oxygen levels for both mother and baby.
🏥 Step 4: Intensive Care Support
- Most patients are transferred to an ICU for:
- Ventilator support
- Heart monitoring
- Ongoing transfusions
- Management of organ failure (if it occurs)
🧘♀️ Recovery and Long-Term Care
- Some survivors may recover fully
- Others may have complications such as:
- Brain damage from lack of oxygen
- Organ damage
- Post-traumatic stress or emotional trauma
- Babies may also experience neurological issues if oxygen was severely limited
🛡️ Can Amniotic Fluid Embolism Be Prevented?
Unfortunately, AFE cannot be fully prevented because it is rare, unpredictable and not well understood. It often occurs suddenly during a normal labor or delivery even without known risk factors.
But there are ways to reduce risk and ensure the best possible outcome through preparedness and risk management.
✅ Risk Reduction Strategies
1. High-Risk Pregnancy Monitoring
- Women with placental problems, multiple pregnancies or a history of AFE should be closely monitored by an obstetrician.
- Specialized care in a hospital with ICU access is recommended.
2. Careful Use of Labor Induction Agents
- Medications like oxytocin or prostaglandins should be used cautiously.
- Overstimulation of the uterus can increase the risk of trauma, which may raise the chance of AFE.
3. Minimize Uterine Trauma
- Avoid unnecessary forceps, vacuum delivery or repeated uterine procedures when possible.
- Be cautious during C-sections or manual placenta removal.
4. Emergency Response Readiness
- Hospitals should have emergency protocols in place for obstetric emergencies like AFE.
- Immediate access to:
- Crash carts
- Trained resuscitation teams
- Blood products and clotting agents
- Quick treatment improves survival significantly.
5. Educating Medical Teams
- Ensure that doctors, nurses and anesthesiologists are trained to:
- Recognize the signs early
- Act fast
- Coordinate emergency interventions
❌ Not Preventable by Lifestyle Changes
- AFE is not caused by diet, exercise or personal habits
- There are no vaccines, supplements or screening tests that can prevent it
🧬 Future Hope: Research and Biomarkers
- Ongoing research is exploring whether certain immune or genetic factors may predict who’s at risk.
- In the future, this might allow for screening or targeted prevention—but we’re not there yet.
📋 Summary:
| Can AFE Be Fully Prevented? | ❌ No, it’s unpredictable and rare |
|---|---|
| Can Risk Be Reduced? | ✅ Yes, with skilled care & readiness |
| Lifestyle Modifiable? | ❌ No |
| Hospital Protocols Matter? | ✅ Critical for survival |
🩷 Real Patient Stories: Amniotic Fluid Embolism
👩🍼 Story 1: Melissa’s Miracle
Location: United States
Situation: Healthy 32-year-old woman, second pregnancy
What Happened:
- Went into labor at full term.
- During the delivery, she suddenly gasped, lost consciousness and went into cardiac arrest.
- Doctors initiated CPR and performed an emergency C-section within minutes.
- Baby was safely delivered, and Melissa was resuscitated but developed severe bleeding (DIC).
- She received multiple blood transfusions and spent a week in the ICU. Outcome: Full recovery after weeks of rehabilitation. Both mom and baby are healthy.
🗨️ “I had no idea what was happening. One minute I was pushing and the next I woke up days later in the ICU.”
👩🍼 Story 2: Sarah’s Silent Warrior
Location: Australia
Situation: First-time mom, no complications during pregnancy
What Happened:
- Suddenly collapsed during early labor.
- Rapid heart failure and breathing distress—diagnosed as AFE.
- Required intubation, emergency delivery and blood products.
- Baby was born with low oxygen levels and spent time in NICU. Outcome: Sarah survived but had mild neurological issues due to oxygen deprivation. Her baby made a full recovery.
🗨️ “I never imagined childbirth could turn into a fight for my life. I’m grateful every single day.”
👩🍼 Story 3: Jessica’s Close Call
Location: Canada
Situation: Scheduled C-section due to breech baby
What Happened:
- Shortly after delivery, Jessica began bleeding uncontrollably.
- Doctors recognized symptoms of DIC and suspected AFE.
- She received over 20 units of blood and was kept sedated in the ICU. Outcome: She survived after 10 days of intensive care. She needed physical therapy to recover but has no lasting damage.
🗨️ “It was terrifying for my family—they were told I might not make it. But the medical team saved my life.”
👩🍼 Story 4: In Loving Memory – A Difficult Truth
Location: United Kingdom
Situation: Third pregnancy
What Happened:
- During a planned C-section, the patient suffered sudden cardiac arrest.
- Despite best efforts, resuscitation failed.
- Baby was delivered but required NICU care due to oxygen deprivation. Outcome: Tragically, the mother passed away from AFE. Baby survived and was later released to the family.
🗨️ Shared by her partner: “She was strong, beautiful, and excited to meet our child. We’ll honor her memory forever.”
We wish a healthy and heappy life to you. You can find helpful advices for tailbone pain during and after pregnancy below:




